news & events
Your UHSP News & Events Hub

Admissions
Strengthening Your College Application: When to Submit Your Test Scores
UHSP campus safety provides 24/7, secure access, trusted partnerships and a close-knit community where every student matters.
Read More

Institutional
Campus Safety at UHSP: What Families Should Know
UHSP campus safety provides 24/7, secure access, trusted partnerships and a close-knit community where every student matters.
Read More
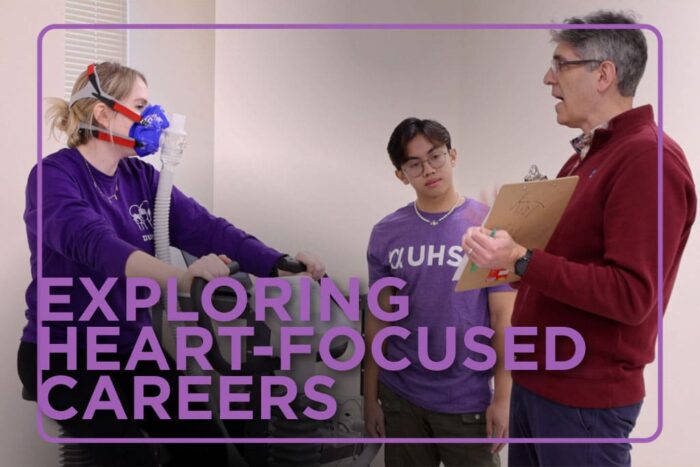
Academics
Heart Smarts: Exploring Heart Health Careers
Discover rewarding heart health career paths, from pharmacists and nurses to exercise physiologists and public health pros.
Read More

Admissions
Three Ways Libraries Help You Succeed in College
Discover ways libraries can help you succeed in college with tech tools, expert librarians and a welcoming space to connect and study.
Read More
Financial Aid
Anatomy of a Financial Aid Package: Understanding College Costs and Aid
Learn the anatomy of a financial aid package, including scholarships, loans, grants and work-study, to prepare for your college journey.
Read More
Financial Aid
College Costs Breakdown: Real Life Scenarios and Financial Aid Options
Get the college costs breakdown with real-life scenarios showing how financial aid components make college more affordable.
Read More
Submit Your Story Ideas
Is there a UHSP story you’d like to be told? We’re always looking for great ideas. Send us your suggestions, and we’ll determine if it can be used for a web story, social media or news media pitch.
Script Magazine
Published twice a year, Script is the University’s alumni publication. Check out the current and past issues for student and alumni profiles, pharmacy and University related features, class notes and general University news.